Murray Luckas MD MRCOG
- Consultant Obstetrician and Gynaecologist, Leighton Hospital,
- Crewe
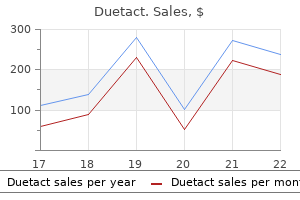
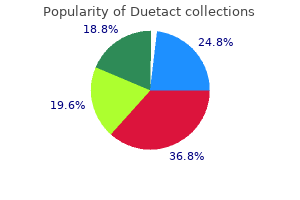
It is converted to as an important organ in controlling the metabo 25-hydroxycholecalciferol in the liver by the addi lism of calcium and phosphate in the body diabetes type 1 vs diabetes mellitus buy duetact 17 mg free shipping. The active vitamin the daily turnover of calcium is represented dia affects: grammatically in Figure 14 metabolic disease you get from ticks buy discount duetact on line. It Because the active metabolites are produced in the restores the calcium level to normal by increasing kidney diabetic diet hummus purchase discount duetact online, renal failure may produce the effects of tubular re-absorption from the kidney and mobi vitamin D de ciency diabetes symptoms skin discount duetact 16 mg with mastercard, and this can only be over lizing calcium from the bones. This hormone is produced by the alternatively, giving the more active metabolites. Cholecalciferol is a fat-soluble these hormonal effects are summarized in vitamin contained in many fatty foods, notably Table 14. Imbalance between them causes either increased or decreased bone Lecture Notes: Orthopaedics and Fractures, 4e. Hormone Mechanism Controlled by Effect Parathyroid hormone Mobilizes Ca2+ from bone Serum calcium ^Serum calcium Increases renal re-absorption of Ca2+ Calcitonin Inhibits bone resorption Serum calcium vSerum calcium Reduces renal re-absorption of Ca2+ Decreases gut absorption of Ca2+ Vitamin D Increases gut Ca2+ absorption Diet ^Serum calcium Changes bone turnover Sunlight Renal function the classi cation below is that suggested by 3 Increase in removal of bone by osteoclasts Aegeter and Kirkpatrick. Bone loss Osteopenia Bone loss (with decreased radiological density and Dietary causes usually thinning of the cortex) can be due to: 1 Decrease in osteoid formation (osteopenia) De cient intake of vitamins or essential proteins 2 Decrease in mineralization of osteoid (osteoma may occur in the malabsorption syndromes, and lacia) or rarely from a true dietary de ciency. This has become rare and only occurs in the fully developed form in children between the ages of 6 Lack of vitamin D or calcium (rickets) Renal tubular acidosis months and 1 year, although old people may have Parathyroid hormone insuf ciency a sub-clinical de ciency. Vitamin C is necessary for collagen synthesis and osteoid deposition, espe cially at the growing ends of bones. Osteogenesis imperfecta Pathological features In the long bones the zone of provisional calci ca See Chapter 9. The epiphysis is ringed with a zone of calci this is a failure of bone mineralization which may cation. Capillaries are abnormally fragile, causing lead to pain, weakness and fragility of the bone. Fractures and epiphyseal displacements are common, and unite with enormous amounts of this is a childhood form of osteomalacia. Dietary de ciency has now become rare except in economically deprived Treatment countries, particularly where there is also de cient Ascorbic acid treatment is rapidly curative. In growing bones the failure of ossi cation leads Endocrine causes to widening of the epiphyseal lines and general ized demineralization. Steroid therapy over a long period may also cause ischaemic necro Clinical features sis of epiphyses, notably the femoral head. The problem in patients who have had organ trans child is small and fails to thrive, developing plants, or other conditions requiring long-term deformities such as bowing of the femora and steroids for immunosuppression, such as in am tibiae, a large head and deformity of the chest with matory arthritis. Investigations Disuse atrophy the serum calcium is usually normal, the phos Bone formation is responsive to mechanical stress, phate is low and the alkaline phosphatase is raised. Renal rickets and vitamin Adult osteomalacia D-resistant rickets the changes are mainly those of softening of the As described above, renal disease may interfere bones. The effects on the growing epiphyses do not with vitamin D metabolism, diminishing the pro apply in the adult so that deformities are not duction of the more active derivatives. The condition is probably more result in malabsorption and abnormal utilization common than is usually thought, particularly in of calcium and phosphate, with secondary parath older people who may have dietary de ciency and yroid stimulation and consequent further dem do not receive suf cient sunlight. In Britain, the condition is commonly found in Certain types of renal tubular insuf ciency may Asian immigrants whose diet may be de cient and result in reduced re-absorption of phosphate, may also encourage calcium de ciency. Large and repeated doses of exacerbations usually in the spine due to crush phosphate may be valuable in the second type. The orthopaedic problems are the same as those 2 Anorexia, weight loss, muscle weakness, some of ordinary rickets, with similar bone deformities times bony deformity. They are well seen in the femoral neck may be useful in renal rickets, vertebral border of the scapula and the ischio although the prognosis for life is poor. Vitamin D in normal doses or, more effectively, a more active metabolite, is usually rapidly curative. Radiological features There is generalized porosis and characteristic localized lesions, which are usually well circum Osteolysis scribed in long bones. These may be widespread or Here, the loss of mineralized bone is due to osteo few in number (Fig. Diagnosis this rests on high serum calcium, low phosphate Hyperparathyroidism and raised alkaline phosphatase. In the primary case, the parathyroid adenoma 2 Secondary hyperparathyroidism, usually in may be excised. Generalized hyperplasia, if it is response to renal disease or as a sequel to osteoma primary, may require removal of two or more of lacia or malabsorption. In primary hyperparathyroidism the serum calcium in blood and urine is raised and phos phate lowered. In secondary hyperparathyroidism calcium may be normal or even low, and phos phate levels vary, depending on the renal pathology. Primary hyperparathyroidism this is characterized by generalized skeletal porosis and the development of cystic lesions lled with soft brown connective tissue. It is most common in old age and particularly in post-menopausal women, although men are not immune. It is de ned as a reduction in bone mineral density as a result of reduced mineral mass, as well as a change in the micro-architecture of the bone itself. Its causes probably include dietary de ciency, lack of stress on bones, both of which cause osteo penia or osteomalacia, and hormonal changes which may act by in uencing the effect of parathy roid hormone and therefore allowing osteolysis. In other words, all the mechanisms of reduction of mineralized bone mass may apply. Clinical features It usually affects women over 60 and to a lesser extent men of the same age. Hip frac Histological features tures in the aged are almost certainly related to the Haversian canals are widened and the trabecu osteoporosis. All patients should be screened biochemically and radiologically to attempt to exclude the speci c disorders listed above. Treatment In typical senile or post-menopausal osteo Treatment and prophylaxis are controversial. It is porosis the X-rays show generalized loss of density usual to give the patient an orthopaedic support of bones and thinning of the cortices from for the spine, to encourage exercise and to give within. Many forms of treatment water are associated with a lower incidence of oste can be shown to in uence the biochemistry of oporosis so uoride therapy has been advocated, osteoporotic patients, but it is dif cult to prove but it has been shown to be associated with a high that they in uence the condition of the bones or incidence of hip fracture. The art of taking a good history lies in eliciting as Financial worries may complicate the situation much relevant information as possible in the and may in uence eventual decisions about treat shortest possible time. It is helpful to get into the habit of making a can be gleaned in a short time, but remember this provisional shortlist of possible diagnoses on the is not the goal but comes with practice. Often in an basis of the symptoms alone, as this helps to direct effort to hurry, the examiner asks leading ques the history taking. Most patients need help to Pain describe their complaints and it is usually best to go through the history in chronological order. Symptoms other than pain may predomi aching, sharp, burning, etc, should be noted and nate. Joint stiffness or instability may be a problem also the degree to which it is aggravated by external and neurological disorders may result in character factors such as walking or straining, as well as its istic functional dif culties. Pain is a symptom and is not conditions are chronic and may result in the the same as tenderness, which is a physical sign.
The vagus nerve Stimulation of the vagus nerve decreases the heart rate childhood diabetes symptoms quiz order cheap duetact on-line, increases smooth muscle tone and mucus secretion in the airways signs getting diabetes purchase 16 mg duetact mastercard, and increases secretion of stomach acid and digestive hormones diabetes type 1 books buy cheap duetact 17mg on-line. Vagal stimulation also decreases the force of cardiac contraction (in contrast with older teaching) blood glucose xls cheap 17mg duetact with mastercard. First, there are parasympathetic ganglia embedded in the myocardium, and vagal stimulation inhibits contraction of myocardial cells. Second, vagal stimulation augments the occupation of inhibitory acetylcholine receptors on sympathetic noradrenergic nerves in the myocardium. The vagus nerve carries afferent traffic to the brain, such as from baroreceptors in the wall of the aorta. The lower part of the parasympathetic nervous system are nerves from the bottom level of the spinal cord, the sacral 67 Principles of Autonomic Medicine v. These nerves travel to the lower gastrointestinal tract, urinary bladder, and genital organs. Vagal parasympathetic innervation of the heart Sacral parasympathetic nerves Sacral parasympathetic stimulation increases peristalsis in the colon and contraction of the rectum while relaxing the anal 68 Principles of Autonomic Medicine v. Such stimulation also increases peristalsis in the ureters and activates the detrusor muscle of the urinary bladder while relaxing the urethral sphincter, so that urination occurs. Parasympathetic stimulation augments filling of the corpora cavernosum and corpus spongiosum of the penis with blood and thereby promotes penile erection. Interference with sacral parasympathetic outflows manifests with constipation, urinary retention, and erectile dysfunction in men. Parasympathetic nervous system failure produces many symptoms, including dry mouth, constipation, urinary problems, decreased tear production, and (in men) inability to have an erection. The nerves of the sympathetic nervous system come from the spinal cord at the levels of the chest and upper abdomen (thoracolumbar spinal cord). The sympathetic nerves to most organs are post-ganglionic, coming from cell bodies in the ganglia, the clusters of nerve cells like a transformer on the utility pole that supplies the electricity to your house. These sub-systems use three different chemical messengers, norepinephrine, acetylcholine, and adrenaline. Actually, this system is always active and participates in many automatic reactions that occur continually, such as tightening of blood vessels in the muscles when you stand up, keeping your glucose level within bounds if you skip a meal, and sweating when you are exposed to a warm environment. The neurotransmitter mediating the ganglionic transmission is acetylcholine acting at nicotinic receptors, and the neurotransmitter released from the post-ganglionic nerve terminals is norepinephrine. Stimulation of the sympathetic noradrenergic system causes the pupils to dilate and the salivary glands to secrete thick saliva. Blood flow is also decreased to the gut, skeletal muscles, and kidneys, and so the 72 Principles of Autonomic Medicine v. It also is an agonist at beta-1 adrenoceptors, but, unlike adrenaline, norepinephrine is a relatively poor agonist at beta-2 adrenoceptors. Its effects in the body are determined mainly by it reaching adrenoceptors before it reaches the bloodstream. The sympathetic adrenergic system plays a major role in responses to perceived or anticipated threats to overall homeostasis, such as lack of essential fuels (glucose and oxygen), inadequate blood flow to vital organs, and hostile encounters. This fits teleologically with the notion of adrenaline being released in sudden emergencies. Adrenaline is secreted into the bloodstream and is distributed widely in the body, so it is a hormone. Norepinephrine and acetylcholine are neurotransmitters, in that they are released from nerve terminals and act locally. Because of stimulation of beta-2 adrenoceptors on vascular smooth muscle cells, adrenaline increases blood flow to skeletal muscle, and probably the systemic cardiovascular effect that occurs at the lowest concentration is a fall in total peripheral resistance. At higher concentrations, adrenaline produces well known stimulation of the heart, increasing both the rate and force of contraction, and constricts blood vessels by stimulating alpha adrenoceptors. Adrenaline also causes pallor, relaxes the gut, increases sweating, increases glucose levels, and increases the core temperature. Failure of the sympathetic adrenergic system might cause a tendency to low glucose levels (hypoglycemia). Because of adrenal blood flowing from the cortex through the 75 Principles of Autonomic Medicine v. The sympathetic cholinergic system consists mainly of non myelinated post-ganglionic nerves to sweat glands. Acetylcholine, the neurotransmitter of the sympathetic cholinergic system, stimulates secretion from sweat glands via muscarinic receptors. The sweat glands also possess adrenoceptors, which when occupied by the neurotransmitter 76 Principles of Autonomic Medicine v. They secrete watery, salty, odorless sweat and are the main mediators of thermoregulatory sweating. Apocrine sweat glands secrete oily, opaque sweat; its characteristic odor results from metabolic breakdown by local bacteria. It is a surprising fact that most of the norepinephrine, dopamine, and serotonin made in the body is synthesized and metabolized in the gut. Autonomic regulation of the stomach involves a complex combination of extrinsic innervation, hormones, autocrine/paracrine factors, and local feedback. For instance, the sympathetic noradrenergic system and the 79 Principles of Autonomic Medicine v. When sympathetic nerves in the heart are stimulated, the heart rate speeds up, and the heart beats more forcefully, whereas when parasympathetic nerves in the heart are stimulated, the heart rate slows down, and the heart beats less forcefully. There are inhibitory muscarinic receptors on sympathetic post ganglionic nerves in the heart. Because of this, vagal stimulation decreases the rate and force of cardiac contraction, not only directly by the released acetylcholine acting at muscarinic receptors on the target myocardial cells but also indirectly by inhibiting norepinephrine release from sympathetic post-ganglionic nerves. In some forms of dysautonomia, multiple components of the autonomic nervous system are affected similarly. For instance, interference with the transmission of nerve impulses in the ganglia produces symptoms and signs of failure of the 80 Principles of Autonomic Medicine v. The sympathetic noradrenergic system and the parasympathetic nervous system usually antagonize each otherbut not always. Overview of autonomic regulation of the cardiovascular system In other situations, increases in activities of these systems go together. In this setting, stimulation of the parasympathetic nervous system aids digestion, by increasing gut motions and augmenting secretion of hormones such as insulin. Meanwhile, stimulation of the sympathetic noradrenergic system tightens blood vessels in particular body regions, shunting blood toward the gut. After a meal, possibly because of increased levels of glucose in the bloodstream, activity of the sympathetic adrenergic system 81 Principles of Autonomic Medicine v. Fainting involves a complex and unusual pattern of changes in activities of components of the autonomic nervous system. When people faint, activity of the parasympathetic nervous system usually is increased, producing changes such as nausea, churning stomach, and a prominent fall in the heart rate. Activity of the sympathetic noradrenergic system often is decreased, resulting in a fall in blood pressure. The sympathetic adrenergic system is stimulated markedly, and high levels of adrenaline in the bloodstream are probably responsible for constriction of blood vessels in the skin, resulting in pallor and dilation of the pupils.
Cheap duetact 16 mg with mastercard. Cure For Diabetes? 5 Revealing Facts Your Doctor Has Missed.
The fasting blood glucose should be checked 3 and 6 months after starting testosterone or after a dose adjustment diabetes 2 purchase cheap duetact line, then annually increase frequency and 338 Hysterectomy monitor A1c if elevated lipids diabetes prevention and control login generic 16 mg duetact mastercard, significant weight gain diabetic beer discount duetact 16 mg visa, elevated fasting glucose levels diabetes insipidus hormone cheap duetact 16 mg without a prescription, personal history of glucose intolerance, or family history of diabetes. Hemoglobin should be checked 3 and 6 months after starting testosterone or after a dose adjustment, then annually. Lipid profile is needed to evaluate 3 and 6 months after starting testosterone or after a dose adjustment, then annually. Liver enzymes also should be checked 3 and 6 months after starting testosterone or after dose increase, then annually. The principal hormonal treatment used to accomplish these goals is testosterone preparation. After reassignment surgery, which includes oophorectomy and hysterectomy, hormonal therapy must be continued. It is reasonable to assume that the principles of treatment are very similar to a person without their own gonadal hormone secretion. An unresolved question is whether in the long term all functions of sex steroids of a subject are adequately covered by cross-sex hormones and whether the administration of cross-sex hormones is appropriate safe. Nearly all hormone related biochemical processes can be sex reversed by administration of cross-sex hormone. Although complications occurring in the long term are seen in general practice, and these complication are only occasionally reported in the scientific literature. Polycythemia and erythrocytosis were observed in testosterone administration as a rare complication[24, 25]. The worrisome complication of water and sodium retention increased body weight, decreased insulin sensitivity, obstructive sleep apnea, acne, poor lipid profile, and an increase in hematocrit have raised the concern for cardiac and thromboembolytic events. Cerebral vascular accidents have been reported for individuals with supraphysiological level of testosterone[27, 28]. Polycystic ovarian disease is a risk factor for endometrial cancer[27] As the association between polycystic ovarian disease and risk of endometrial and ovarian malignancy are not entirely clear and seen in greater numbers in transsexual people before androgen therapy than in the general population[28, 29]. Recommendation for hysterectomy and bilatel salpingoooporectomy, generally carried out around 15 months after the start of testosterore treatment in the male to female transsexuals, has yet to be fully justified, at least on the grounds of enhanced risk of malignancy. Total hysterectomy after 2 years of testosterone therapy, followed by 50% reduction in hormone man be a way to avoid these risks[32, 33](Table 2). Know-How of the Hormonal Therapy and the Effect of the Male Hormone on Uterus in the Female to Male Transsexuals 339 1. The effect of the testosterone on uterus and ovary Human endometrium is a steroid-hormone-dependent tissue whose growth and remodeling respond to estrogen and progesterone secreted from ovary. Testosterone treatments to the female to male transsexuals are a usual method to induce masculinization. Testosterone is one of the potent circulating androgens which are produced from testis and ovary. Ovary and adrenal gland in women produce not only female sex hormones and mineralcorticoid, but also androgens, such as testosterone, androstenedione and dehydroepiandrostenedione or its sulfate. Several studies have shown that high plasma androgen levels are associated with adverse reproductive outcome, including infertility and increased incidence of miscarriage. Although it is easily acceptable that there are no definite gross changes of uterus and ovary, interesting histological features are expressed in a few articles. In the study, severe atrophied uterine cervix was found and variable degrees of atrophic change of endometrium were observed as well. Finally, it is concluded that the histolgic changes of endometrium and ovary are atrophic and polycystic appearance according to the duration of testosterone treatments. Atrophied epithelium of exocervix (H-E, X400) (Kor J Fertil Steril 2005;32:325-330) Know-How of the Hormonal Therapy and the Effect of the Male Hormone on Uterus in the Female to Male Transsexuals 341 Fig. Multiple cystic follicles in the ovarian cortex (H-E, X10) (Kor J Fertil Steril 2005;32:325 330) 342 Hysterectomy 7. Conclusions the use of hormonal therapy in transsexualism is associated with appropriate physical change. Side effects in carefully monitored patients are usually few but are more likely to cause serious complications when therapy is too aggressive. Investigators propose that initial treatment with androgen therapy which must be supraphysiological to suppress gonadotropins and virilize the patient should be kept to maximum of no more than 2 years. Following sex reassignment surgery, the dosage should be reduced by half in most patients. It is likely to reduce not only the duration of large dosage androgen therapy but also the potential risk of endometrial hyperplasia and uterine carcinoma. The role of the concerned physician is to be fully aware of potential risk of this therapy so as to adjust treatment and minimize potential complications. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. Venereology: Interdisciplinary, International Journal of Sexual Health, 10, 175-177. Effects of sex steroid hormones on regional fat depots as assessed by magnetic resonance imaging in transsexuals. Endocrine therapy of transsexualism and potential complications of long-term treatment. Transgender care: Recommended guidelines, practical information, and personal accounts. Long-Term Treatment of Transsexuals with Cross-Sex Hormones: Extensive Personal Experience. Horm Res, 64(2), 31-36 [23] Vancouver Coastal Health, Transcend Transgender Support & Education Society, and the Canadian Rainbow Health Coalition. Endocrine therapy for transgender adults in British Columbia: Suggested guidelines. Serum androgen levels in women who suffer recurrent miscarriage and their correlation with markers of endometrial function. Polycystic ovaries and levels of gonadotrophins and androgens in recurrent miscarriage: prospective study in 50 women. Ultrasound and menstrual history in predicting endometrial hyperplasia in polycystic ovary syndrome. The Histologic Features of the Uterus and Adnexa Extirpated from Gender Identity Disorder Patients with Depot Androgen Injection. The first report of prophylactic oophorectomy for familial ovarian cancer was in 1950 when A. M Liber described a family of five sisters and their mother, all with histologically confirmed papillary adenocarcinoma of the ovary; it was recommended that family members should undergo frequent gynaecologic screening, and that prophylactic oophorectomy should be considered (Liber, 1950) the role of oophorectomy in the management of breast cancer dates further back to 1889 when it was first proposed by Albert Schinzinger (Schinzinger, 1889); he observed that the prognosis for breast cancer appeared better in older women than younger women and postulated that oophorectomy would initiate atrophy of the breast and any cancer within the breast. Shinzinger suggested oophorectomy both as therapy for advanced breast cancer and prophylaxis against local recurrence, but he never actually performed the surgery; it was George Thomas Beatson who first performed a bilateral oophorectomy on a patient with metastatic breast cancer in 1895, this was reported in the Lancet in 1896 (Beatson, 1896). A subsequent report detailed that this patient experienced remission of her disease and lived another four years. Beatson hypothesized that oophorectomy caused fatty degeneration of the malignant cells accounting for its beneficial effect in breast cancer (Beatson, 1896; Thomson, 1902). An English surgeon, Stanley Boyd performed the first oophorectomy as adjuvant breast cancer therapy in 1897 (Boyd, 1897). In 1968 Feinleib observed that 346 Hysterectomy premenopausal oophorectomy decreased the rate of subsequent breast cancer (Feinleib, 1968) however it was a further twenty years before Brinton proposed the potential of oophorectomy as a breast cancer prevention strategy, reporting that women, with a family history of breast cancer, who underwent oophorectomy before the age of 40 years had a 45% reduction in breast cancer risk compared with women who underwent natural menopause (Brinton et al, 1988). Meijer and van Lindert similarly reported that surgery performed before the age of natural menopause significantly reduced breast cancer risk (Meijer & van Lindert, 1992). This milestone in breast and ovarian cancer research was one of the most significant cancer discoveries of the twentieth century, both in terms of scientific impact and public interest. However there are specific populations in which the frequency of mutations are higher due to strong founder effect; these include ethnic and geographic populations worldwide including those of Norwegian, Dutch and Icelandic descent (Neuhausen et al, 2009).
Neurodegeneration with brain iron accumulation: clinical diabetes mellitus type 2 hla order duetact 17mg without a prescription, radiographic and genetic heterogeneity and corresponding therapeutic options diabetes type 1 yeast infections generic duetact 17mg line. Bilateral Subthalamic Nucleus Stimulation in the Treatment of Neurodegeneration with Brain Iron Accumulation Type 1 diabetic food purchase duetact with visa. Postanoxic generalized dystonia improved by bilateral Voa thalamic deep brain stimulation diabetes weight loss buy cheapest duetact and duetact. Interruption of deep brain stimulation of the globus pallidus in primary generalized dystonia. Long-term outcome of bilateral pallidal deep brain stimulation for primary cervical dystonia. Pallidal stimulation for pantothenate kinase associated neurodegeneration dystonia. Outcome predictors of pallidal stimulation in patients with primary dystonia: the role of disease duration. Pallidal deep brain stimulation in primary cervical dystonia with phasic type: clinical outcome and postoperative course. Bilateral pallidal deep brain stimulation in a case of myoclonus dystonia syndrome. Long term benefit to pallidal deep brain stimulation in a case of dystonia secondary to pantothenate kinase associated neurodegeneration. Myoclonus and tremor response to thalamic deep brain stimulation parameters in a patient with inherited myoclonus-dystonia syndrome. Deep brain stimulation as a mode of treatment of early onset pantothenate kinase-associated neurodegeneration. Neue stereotaktisch-functionelle Behandlungsmethode des Torticollis spasmodicus mit Hirn-stimulatoren. Differential Response of Dystonia and Parkinsonism following Globus Pallidus Internus Deep Brain Stimulation in X Linked Dystonia-Parkinsonism (Lubag). A prospective blinded evaluation of deep brain stimulation for the treatment of secondary dystonia and primary torticollis syndromes. Long term clinical outcome in Meige syndrome treated with internal pallidum deep brain stimulation. Neurostimulation of the ventral intermediate thalamic nucleus in inherited myoclonus dystonia Syndrome. Bilateral pallidal deep brain stimulation for the treatment of patients with dystonia-choreoathetosis cerebral palsy: a prospective pilot study. Use of surface electromyography to assess and select patients with idiopathic dystonia for bilateral pallidal stimulation. Increased risk of lead fracture and migration in dystonia compared with other movement disorders following deep brain stimulation. Stimulation-induced parkinsonism after posteroventral deep brain stimulation of the globus pallidus internus for craniocervical dystonia. Introduction Cervical dystonia is the most common form of focal dystonia (Dashtipour et al. It is characterized by involuntary movement of the neck resulting in abnormal neck posture (Brin & Benabou, 1999; Dent, 2002). Cervicalgia and headache sometimes occur in patients suffering from the disease (Albanese, 2005; Brashear, 2004, Schim, 2006). A critical long-term sequelae of this kind of movement disorder is premature cervical spinal degenerative disease (Chawda et al. Fundamentally, cervical dystonia is categorized into several patterns, including torticollis (head rotation), anterocollis (head forward flexion), retrocollis (head backward extension), laterocollis (lateral head bending), and combined pattern (Brin & Benabou, 1999; Feely, 2003; Sitthinamsuwan & Nunta-aree, 2010; Sitthinamsuwan et al. For instance, involved muscles in torticollis include the posterior cervical muscles (mainly splenius capitis, semispinalis capitis and semispinalis cervicis) on the same side of turning head and the contralateral sternocleidomastoid. The various dystonic patterns and corresponding neck muscles are summarized in Fig. Conventional treatment of cervical dystonia consists of oral medication, botulinum toxin injection, and physical therapy. For patients who do not respond to such therapies or are refractory cases, surgical treatment is an appropriate option (Nunta-aree & Sitthinamsuwan, 2009; Nunta-aree et al. Surgical therapy for cervical dystonia has been continuously developed for a significant period to improve outcome and diminish complication. Some operations have been abandoned because of their potential complications while some of them have been used increasingly and are currently popular on account of their effectiveness and safe (Albanese, 2005; Albanese et al. Overview of surgical treatment for cervical dystonia is described in the following. Dystonia and Peripheral Nerve Surgery in the Cervical Area 153 a) Intradural anterior cervical rhizotomy Originally, bilateral C1-C3 anterior spinal nerve roots were resected intradurally in this operation (Munchau et al. A significant numbers of patient developed swallowing dysfunction following the surgery while improvement of cervical dystonia was not appreciable. Consequently, there is no use of bilateral C1-C3 anterior rhizotomy in the present (Brin & Benabou, 1999; Bronte-Stewart, 2003; Taira, 2009). However, recently, intradural C1-C2 anterior rhizotomy has been successfully combined with selective denervation of C3-C6 posterior rami successfully without serious adverse effect (Taira et al. It sometimes caused respiratory insufficiency as a result of diaphragmatic dysfunction (Fraioli et al. Nowadays, posterior rhizotomy in the cervical level are performed only on C5 to T1 posterior nerve spinal roots and it aims to treat bilateral upper limb spasticity (Benedetti et al, 1977; Bertelli et al. It affected not only motor fibers to the sternocleidomastoid but also those to the trapezius. Postoperative trapezius atrophy and shoulder instability inevitably occurred (Bronte-Stewart, 2003; Sorensen & Hamby 1965). Bilateral procedures, however, commonly resulted in speech disturbance (Bronte-Stewart, 2003; Imer et al. Nevertheless, the hypothesis of accessory nerve decompression cannot explain improvement of cervical dystonia in the individuals who have no dystonia of both the muscles (Albanese et al. Good to excellent outcome is often achieved by the operation, so it has become a common surgical treatment for cervical dystonia (Albanese, 2005; Albanese et al. This type of surgery is the central idea of the present chapter and its content will be stated in detail. In the authors view, muscle section is an adjunctive procedure for cervical dystonia and should be considered in cases with long standing dystonia which exhibit evidence of soft tissue stiffness or muscle shortening. Furthermore, it may be performed on muscles which are difficult to denervate (Ondo & Krauss, 2004), such as the scalene muscles. However, among our patients with uncomplicated or simple cervical dystonia, we did not encounter substantial difference of outcome between the patients who underwent pallidal deep brain stimulation and those who underwent peripheral denervation. Therefore, we always chose peripheral nerve resection as the primary surgical therapy in the uncomplicated cases. On the other hand, we consider the deep brain stimulation as the prerequisite treatment of complex cervical dystonia, such as mobile cervical dystonia, segmental dystonia, head tremor, anterocollis, severe retrocollis, in the patients who have significant extracervical symptoms, or who have never been improved by botulinum toxin injection (primary botulinum toxin non-responder). Such complicated cases are always difficult to deal with through selective peripheral denervation (Albanese et al. However, currently, it appears to be a good surgical option in various pain disorders, particularly in neuropathic pain and pain of ischemic origin (Forouzanfar et al. This chapter focuses on peripheral nerve surgery in the cervical region for cervical dystonia which refers to selective peripheral denervation in terms of patient selection, preoperative evaluation, operative procedures with relevant surgical anatomy, and surgical outcome. Patient selection Selective peripheral denervation is chiefly indicated in patients with failed botulinum toxin injection, including those who have never responded to the injection (primary botulinum toxin non-responder) or who have a change from significant previous response to poor recent response (secondary botulinum toxin non-responder) (Albanese et al. Good surgical candidates for the operation include those who meet the following parameters (Braun et al.