Cindy L. O�Bryant, PharmD, BCOP
- Associate Professor, Department of Clinical Pharmacy, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences
- Clinical Pharmacy Specialist, University of Colorado Cancer Center, Aurora, Colorado
http://www.ucdenver.edu/academics/colleges/pharmacy/Departments/ClinicalPharmacy/DOCPFaculty/H-P/Pages/OBryantCindyPharmD.aspx
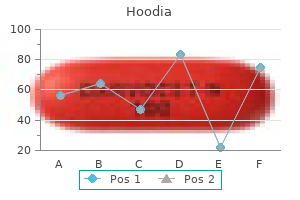
For all these index values herbals on demand coupon order hoodia pills in toronto, the intertwin differences (delta value) were determined by subtracting the values obtained in the larger twin from those of the smaller twin herbals names order on line hoodia. In the dichorionic pregnancies herbs like kratom hoodia 400mg low price, there were significant changes of delta values for all the parameters tested xena herbals buy hoodia master card. Similarly, delta values of peak velocity from outflow tracts significantly decreased, whereas those of the percentage reverse flow in the inferior vena cava increased. It was concluded that serial Doppler recordings may show hemodynamic changes in the fetal circulation of discordant twins. Different trends occur according to the underlying pathophysiological mechanisms of the growth defect. Doppler investigations of the arterial vessels and ductus venosus, inferior vena cava, right hepatic vein, tricuspid and mitral ventricular inflow were performed in both fetuses. Mean values of most blood flow velocities on the venous side showed a significant decrease in both groups of fetuses, and a significant increase in mean values for indices describing waveform pulsatility was found in all three venous vessels in the group of recipients, whereas, in the donor group, this was only the case in the ductus venosus. Mean values of atrioventricular flow velocities showed a significant decrease in the donor group. Five recipients and four donors had absence or reversal of blood flow during atrial contraction in the ductus venosus. Absence or reversal of end-diastolic velocities in the umbilical artery was found in four donors. The circulation of the recipient showed the characteristics of congestive heart failure due to hypovolemia. The significant decrease of diastolic venous blood flow velocities is compatible with increased end-diastolic ventricular pressure. Alterations in the circulation of the donor are consistent with decreased venous return due to hypovolemia and increased cardiac afterload due to increased placental resistance. One recipient twin died a week after delivery of endocardial fibroelastosis and infundibular pulmonary stenosis. Two others had balloon dilatation for pulmonary stenosis, one shortly after birth and one at 4 months. Figure 4: Pulsations in the umbilical vein with reversal of flow at the end of diastole in the recipient fetus of a pregnancy with twin-to-twin transfusion syndrome Figure 5: Holosystolic tricuspid regurgitation in the recipient fetus of a pregnancy with twin-to-twin transfusion syndrome Hecher et al. Fetoscopic laser coagulation of the placental anastomoses was performed at 20 weeks of gestation. Subsequently, there was evidence of increased placental vascular resistance in the donor twin and major impairment of right ventricular function, with no forward flow through the tricuspid valve. During the next 4 weeks, however, there was spontaneous and complete recovery of ventricular function and resolution of the functional tricuspid valve atresia. These findings suggest that alterations in fetal hemodynamics may result in structural cardiac abnormality and may be the precursors of some forms of congenital heart disease. Intertwin comparisons were made for the following cardiac parameters: cardiothoracic index, end-diastolic thickness of the ventricular walls and septum, aortic and pulmonary artery Doppler peak velocities, ejection and acceleration times, left ventricular shortening fraction, and combined cardiac output and output indexed to fetal weight. The left ventricular shortening fractions and outputs were significantly increased in the donor twin with twin-to-twin transfusion syndrome and normal in placental insufficiency. It was concluded that, in twin-to-twin transfusion syndrome, the donor twin shows evidence of a hyperdynamic cardiac state. Intertwin comparison of cardiac parameters, especially the left ventricular shortening fraction, can be considered a useful tool in diagnosing the different etiologies of the polyhydramnios oligohydraminos sequence. Serial Doppler echocardiographic sudies showed no specific cardiac involvement in the donor twins, either in utero or after birth. In contrast, all recipient twin fetuses showed variable degrees of biventricular hypertrophy and dilatation with tricuspid regurgitation. Deterioration in the fetal condition is associated with a breakdown of hemodynamic compensatory mechanisms, with a decline in cardiac output and the development of abnormal venous flow with increase in pulsatility of ductus venosus waveforms and loss of forward flow velocity during atrial contraction. In monochorionic twins with no twin-to-twin transfusion syndrome, the incidence of vascular anastomoses is much higher than in those with the syndrome. Additionally, there is decreased blood flow velocity and increased impedance to flow in the ductus venosus of both the donor and recipient fetuses. In donor fetuses, flow velocities across the atrioventricular valves are decreased. In the recipient, there is evidence of hypervolemia with congestive heart failure; hypervolemia may cause compensatory cardiac hypertrophy, but eventually the pumping capabilities of the enlarged heart are exceeded and cardiac failure occurs. The lambda sign at 10?14 weeks of gestation as a predictor of chorionicity in twin pregnancies. The contribution of singletons, twins and triplets to low birth weight, infant mortality and handicap in the United States. Therapeutic amniocentesis in twin?twin transfusion syndrome appearing in the second trimester of pregnancy. Monoamniotic twins: improved perinatal survival with accurate prenatal diagnosis and antenatal fetal surveillance. Early prenatal diagnosis of cord entanglement in monoamniotic multiple pregnancies. Abundant vascular anastamoses in monoamniotic versus diamniotic monochorionic placentas. Discordant twins a prospective study of the diagnostic value of real-time ultrasonography combined with umbilical artery velocimetry. Prediction of the small for gestational age twin fetus by Doppler umbilical artery waveform analysis. Is pulsed Doppler velocimetry useful in the management of multiple-gestation pregnancies? Doppler flow velocity waveforms in fetal surveillance of twins: a prospective longitudinal study. Placental microvascular changes in twin pregnancies with abnormal umbilical artery waveforms. Color Doppler ultrasonography in the identification of communicating vessels in twin?twin transfusion syndrome and acardiac twins. Colour Doppler energy insonation of placental vasculature in monochorionic twins: absent arterio?arterial anastomoses in association with twin-to-twin transfusion syndrome. The value of Doppler ultrasound in the diagnosis and management of twin-to-twin transfusion syndrome. Doppler velocimetry determined redistribution of fetal blood flow: correlation with growth restriction in diamniotic monochorionic and dizygotic twins. Clinical and echographic features of in utero cardiac dysfunction in the recipient twin in twin?twin transfusion syndrome. Temporary iatrogenic fetal tricuspid valve atresia in a case of twin to twin transfusion syndrome. Potential value of fetal echocardiography in the differential diagnosis of twin pregnancy with presence of polyhydramnios oligohydramnios syndrome. The two methods are complementary to each other, with color Doppler being used for general assessment of flow in the region of interest and pulsed Doppler for targeted examination of flow in a vessel or across a valve 1-10. In pulsed Doppler ultrasound, the examiner positions a sample volume over the region of interest to obtain flow velocity waveforms as a function of time. This makes it possible to quantify blood flow as peak or time-averaged mean velocities, which allow the calculation of ratios (such as the E/A ratio) or blood volume (such as stroke volume or cardiac output) after measurement of vessel diameter. Color Doppler, which is technically easier to perform, allows a rapid assessment of the hemodynamic situation, but gives only descriptive or semi-quantitative information on blood flow. Color Doppler should be an integral part of the routine examination of a fetal heart because this helps to shorten the scanning time, but also provides improved reliability in diagnosing or excluding abnormalities. Several planes, including the abdominal view, four-chamber view, five-chamber view, the short-axis and the three-vessel view need to be assessed to achieve spatial information on different cardiac chambers and vessels as well as their connections to each other 1,2,4. The difference from two-dimensional scanning is that, with color Doppler, the angle of insonation should be as small as possible for optimal visualization of flow. In the abdominal plane, the position of the aorta, inferior vena cava and the connection of the vein to the right atrium are examined. Pulsed Doppler sampling from the inferior vena cava, the ductus venosus or the hepatic veins can be achieved in longitudinal planes. Using color Doppler in an apical (Figure 1) or basal approach, the diastolic perfusion across the atrioventricular valves can be assessed; there is a characteristic separate perfusion of both inflow tracts during diastole (Figure 1). Using pulsed Doppler, there is a typical biphasic shape of the diastolic flow velocity waveform with an early peak diastolic velocity (E) and a second peak during atrial contraction (A-wave); E is smaller than A, and the E : A ratio increases during pregnancy toward 1, to be inversed after birth. In this plane, regurgitation across the atrioventricular valves, which is more frequent at the tricuspid valve, is easily detected during systole with color Doppler. Flow across the foramen ovale is visualized in a lateral approach of the four-chamber view.
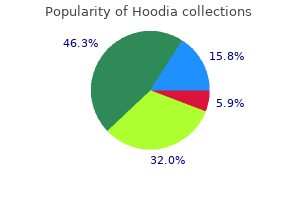
As a result of this prioritization greenwood herbals 400mg hoodia free shipping, there were fewer reviews completed in 2015 (166) than in 2010 (274) herbals and surgery order hoodia 400 mg with mastercard. Distribution of Classes of Once the topics were selected herbs names buy 400 mg hoodia fast delivery, there were 2 important Recommendation and Levels of additions to the 2015 process of review itself herbals soaps buy cheap hoodia 400mg line. There is greater awareness that although children and As resuscitation practice evolves, ethical considerations adolescents cannot make legally binding decisions, must also evolve. The patient is ultimately transferred to procedures) that, when integrated, produce a system (eg, a critical care unit for continued care. Recommendations have been strengthened to encourage is still evolving, there is face validity in the concept of having immediate recognition of unresponsiveness, activation of the teams trained in the complex choreography of resuscitation. The recommended chest compression rate is 100 to 120/min should systematically monitor cardiac arrests, the level of (updated from at least 100/min). The clarifed recommendation for chest compression depth for adults feedback, measurement or benchmarking, and analysis. Bystander-administered naloxone may be considered for suspected care so that the gaps between ideal and actual resuscitation life-threatening opioid-associated emergencies**. Legally, a prescribed drug may only be administered to the person named on the prescription, not a third party. More Cardiac arrest victims sometimes present with seizure-like information about these changes appears below. Thus, immediate access to role that emergency dispatchers can play in helping the lay a defbrillator is a primary component of the system of care. All lay in municipal buildings, large public venues, airports, casinos, rescuers should, at a minimum, provide chest compressions and schools. All trained lay rescuers should, at a minimum, prearrival dispatch protocols, can improve outcomes. In most studies, more compressions are breaths, compressions and breaths should be provided in a associated with higher survival rates, and fewer compressions ratio of 30 compressions to 2 breaths. The addition of an lay rescuer who is able, the recommendation remains for the upper limit of compression rate is based on 1 large registry rescuer to perform both compressions and breaths. Chest Compression Rate* Box 1 uses the analogy of automobile travel to explain the 2015 (Updated): In adult victims of cardiac arrest, it is effect of compression rate and interruptions on total number of reasonable for rescuers to perform chest compressions at a compressions delivered during resuscitation. Rescuers often do not compress the chest deeply enough despite the recommendation to push Number of Compressions Delivered hard. Compression depth may the total number of compressions delivered during resuscitation is an be diffcult to judge without use of feedback devices, and important determinant of survival from cardiac arrest. Increases in compression rate and fraction between excessive compression depth and injuries that increase the total number of compressions delivered. When traveling in an automobile, the number of miles traveled in a day is affected not only by Bystander Naloxone in Opioid-Associated Life the speed (rate of travel) but also by the number and duration of any Threatening Emergencies* stops (interruptions in travel). Traveling 60 mph without interruptions translates to an actual travel distance of 60 miles in an hour. Traveling 60 2015 (New): For patients with known or suspected mph except for a 10-minute stop translates to an actual travel of 50 opioid addiction who are unresponsive with no normal miles in that hour. The more frequent and the more prolonged the stops, breathing but a pulse, it is reasonable for appropriately the lower the actual miles traveled. This topic is also addressed in the Special Circumstances of Resuscitation section. This simplifed ventilation rate of 1 breath every 6 seconds (10 breaths recommendation incorporates the newly approved treatment**. For example, provider, especially if acting alone, should still be to activate the proportion of compressions of inadequate depth was the emergency response system and to provide chest about 35% for a compression rate of 100 to 119/min compressions. Chest Compression Rate: 100 to 120/min* Minimizing Interruptions in Chest 2015 (Updated): In adult victims of cardiac arrest, it is Compressions* reasonable for rescuers to perform chest compressions at a 2015 (Reaffrmation of 2010): Rescuers should attempt to rate of 100 to 120/min. Three studies Why: Interruptions in chest compressions can be intended in systems that use priority-based, multitiered response in as part of required care (ie, rhythm analysis and ventilation) both urban and rural communities, and provide a bundled or unintended (ie, rescuer distraction). Chest compression package of care that includes up to 3 cycles of passive fraction is a measurement of the proportion of total oxygen insuffation, airway adjunct insertion, and 200 resuscitation time that compressions are performed. An continuous chest compressions with interposed shocks, increase in chest compression fraction can be achieved by showed improved survival with favorable neurologic status minimizing pauses in chest compressions. Since the 2010 continuous compressions with passive oxygen insuffation Guidelines were published, a number of clinical trials have and airway adjuncts. Activate emergency response breathing, Look for no breathing breathing, system (if not already done) Monitor until has pulse or only gasping and check has pulse after 2 minutes. The load-distributing band When rescuers or healthcare systems are considering may be considered for use by properly trained personnel in implementation, it must be noted that some techniques and specifc settings for the treatment of cardiac arrest. Manual chest compressions remain the standard of care for the treatment of cardiac arrest. Also, vasopressin does not offer an advantage over the use of 2010 (Old): Mechanical piston devices may be considered epinephrine alone. Therefore, to simplify the algorithm, vasopressin for use by properly trained personnel in specifc settings for has been removed from the Adult Cardiac Arrest Algorithm the treatment of adult cardiac arrest in circumstances (eg, 2015 Update. Vasopressors for Resuscitation: Vasopressin Post?Cardiac Arrest Drug Therapy: Lidocaine 2015 (Updated): Vasopressin in combination with epinephrine 2015 (New): There is inadequate evidence to support the offers no advantage as a substitute for standard-dose routine use of lidocaine after cardiac arrest. Review of the available evidence shows that effcacy of the 2 drugs is similar and that there is no demonstrable beneft Post?Cardiac Arrest Drug Therapy:? In the interest of 2015 (New): There is inadequate evidence to support the simplicity, vasopressin has been removed from the Adult routine use of a? However, this fnding is only an associative relationship, and the Why: A very large observational study of cardiac arrest with routine use of? Therefore, providers should evaluate an association between early administration of epinephrine patients individually for their suitability for? Identifcation and correction of hypotension is recommended in the management at 36?C and at 33?C and found outcomes to immediate post?cardiac arrest period. All patients who progress to brain death or circulatory death after clinical factors. Coronary angiography is reasonable in post?cardiac with harm, preventing fever is suggested. It had been assumed that earlier initiation of cooling might provide added benefts Why: Multiple observational studies found positive and also that prehospital initiation might facilitate and associations between emergency coronary revascularization encourage continued in-hospital cooling. Because the outcome of coma Hemodynamic Goals After Resuscitation may be improved by correction of cardiac instability, and the prognosis of coma cannot be reliably determined in the frst 2015 (New): It may be reasonable to avoid and immediately few hours after cardiac arrest, emergency treatment of post correct hypotension (systolic blood pressure less than 90 cardiac arrest patients should follow identical guidelines. In addition, the comatose brain systolic blood pressure less than 90 mm Hg or a mean arterial may be more sensitive to medications, and medications may pressure of less than 65 mm Hg is associated with higher take longer to metabolize after cardiac arrest. While higher pressures appear superior, recovery after cardiac arrest with 100% certainty. Multiple specifc systolic or mean arterial pressure targets could not modalities of testing and examination used together to be identifed, because trials typically studied a bundle of many predict outcome after the effects of hypothermia and interventions, including hemodynamic control. Also, because medications have been allowed to resolve, are most likely to baseline blood pressure varies from patient to patient, different provide accurate prediction of outcome (Box 2). Organ Donation 2015 (Updated): All patients who are resuscitated from Prognostication After Cardiac Arrest cardiac arrest but who subsequently progress to death 2015 (New): the earliest time to prognosticate a poor or brain death should be evaluated as potential organ neurologic outcome using clinical examination in patients donors. Starting with this update, recommendations will be limited to the prehospital and emergency department That Are Associated With phases of care. There is, however, no evidence of mortality beneft of one therapy over 2010 (Old): If biomarkers are initially negative within 6 hours the other. Opioid Overdose Education and Naloxone Moreover, adding medications increases the complexity of Training and Distribution prehospital care, which may in turn produce negative effects. Special Circumstances Cardiac Arrest in Patients With Known or of Resuscitation Suspected Opioid Overdose 2015 (New): Patients with no defnite pulse may be in Summary of Key Issues and Major Changes cardiac arrest or may have an undetected weak or slow pulse. In addition, a new algorithm for management of the possibility that the patient is in respiratory arrest, not unresponsive victims with suspected opioid overdose is provided. While there is no evidence that administration of naloxone will help a patient in cardiac 18 American Heart Association Figure 6 Opioid-Associated Life-Threatening Opioid-Associated Life-Threatening Emergency (Adult) Algorithm?New 2015 Emergency (Adult) Algorithm Assess and activate. Continue to check responsiveness and Yes At any time, does the person breathing until advanced help arrives.
Partial mastectomy procedures are reported using codes 19301 or 19302 as appropriate herbs list generic 400mg hoodia amex. Documentation for partial mastectomy procedures includes attention to the removal of adequate surgical margins surrounding the breast mass or lesion herbs during pregnancy purchase hoodia 400mg visa. Version 2019 Page 26 of 257 Physician Procedure Codes zip herbals buy hoodia 400 mg lowest price, Section 5 Surgery Total mastectomy procedures include simple mastectomy vedantika herbals hoodia 400 mg overnight delivery, complete mastectomy, subcutaneous mastectomy, modified radical mastectomy, radical mastectomy, and more extended procedures (eg, Urban type operation). Excisions or resections of chest wall tumors including ribs, with or without reconstruction, with or without mediastinal lymphadenectomy, are reported using codes 19260, 19271, or 19272. Codes 19260-19272 are not restricted to breast tumors and are used to report resections of chest wall tumors originating from any chest wall component. The services listed below include the application and removal of the first cast or traction device only. Subsequent replacement of cast and/or traction device may require an additional listing. This terminology is used to describe procedures that treat fractures by three methods: 1) without manipulation; 2) with manipulation; or 3) with or without traction. In this procedure, the fracture fragments are not visualized, but fixation (eg, pins) is placed across the fracture site, usually under x-ray imaging. The type of fracture (eg, open, compound, closed) does not have any coding correlation with the type of treatment (eg, closed, open or percutaneous) provided. The codes for treatment of fractures and joint injuries (dislocations) are categorized by the type of manipulation (reduction) and stabilization (fixation or immobilization). These codes can apply to either open (compound) or closed fractures or joint injuries. Skeletal traction is the application of a force (distracting or traction force) to a limb segment through a wire, pin, screw or clamp that is attached (eg, penetrates) to bone. Skin traction is the application of a force (longitudinal) to a limb using felt or strapping applied directly to skin only. External fixation is the usage of skeletal pins plus an attaching mechanism/device used for temporary or definitive treatment of acute or chronic bony deformity. Codes for obtaining autogenous bone grafts, cartilage, tendon fascia lata grafts or other tissues, through separate incisions are to be used only when the graft is not already listed as part of the basic procedure. Re-reduction of a fracture and/or dislocation performed by the primary physician may be identified by either the addition of the modifier -76 to the usual procedure number to indicate Repeat Procedure by Same Physician. To report, list only the primary surgical procedure performed (eg, sequestrectomy, deep incision). These codes describe surgical exploration and enlargement of the wound, extension of dissection (to determine penetration), debridement, removal of foreign body(s), ligation or coagulation of minor subcutaneous and/or muscular blood vessel(s), of the subcutaneous tissue, muscle fascia, and/or muscle, not requiring thoracotomy or laparotomy. If a repair is done to major structure(s) or major blood vessel(s) requiring thoracotomy or laparotomy, then those specific code(s) would supersede the use of codes 20100 20103. To report Simple, Intermediate or Complex repair of wound(s) that do not require enlargement of the wound, extension of dissection, etc. Codes 21076-21089 should only be used when the physician actually designs and prepares the prosthesis (ie, not prepared by an outside laboratory). For bone grafts in other Musculoskeletal sections, see specific code(s) descriptor(s) and/or accompanying guidelines. Example: Posterior arthrodesis of L5-S1 for degenerative disc disease utilizing morselized autogenous iliac bone graft harvested through a separate fascial incision. To report instrumentation procedures performed with definitive vertebral procedure(s), see codes 22840 22855,22859. Instrumentation procedure codes 22840-22848,22853,22854,22859 are reported in addition to the definitive procedure(s). The modifier 62 may not be appended to the definitive add-on spinal instrumentation procedure code(s) 22840 22848, 22850,22852,22853,22854,22859. Example: Posterior arthrodesis of L4-S1, utilizing morselized autogenous iliac bone graft harvested through separate fascial incision, and pedicle screw fixation. Vertebral procedures are sometimes followed by arthrodesis and in addition may include bone grafts and instrumentation. When arthrodesis is performed addition to another procedure, the arthrodesis should be reported in addition to the original procedure. Examples are after osteotomy, fracture care, vertebral corpectomy and laminectomy. Since bone grafts and instrumentation are never performed without arthrodesis, they are reported as add-on codes. Example: Treatment of a burst fracture of L2 by corpectomy followed by arthrodesis of Ll-L3, utilizing anterior instrumentation Ll-L3 and structural allograft. In this situation, the modifier 62 may be appended to the procedure code(s) 22100-22102, 22110-22114 and, as appropriate, to the associated additional vertebral segment add-on code(s) 22103, 22116 as long as both surgeons continue to work together as primary surgeons. In this situation, the modifier 62 may be appended to code(s) 22210-22214, 22220-22224 and, as appropriate, to associated additional segment add-on code(s) 22216, 22226 as long as both surgeons continue to work together as primary surgeons. In this situation, the modifier 62 may be appended to code(s) 22318-22327, and, as appropriate, to associated additional segment add-on code 22328 as long as both surgeons continue to work together as primary surgeons. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies, which contains the intervertebral disc, and includes the nucleus pulposus, annulus fibrosus, and two cartilagenous endplates. For the following codes, when two surgeons work together as primary surgeons performing distinct part(s) of an anterior interbody arthrodesis, each surgeon should report his/her distinct operative work by appending the modifier 62 to the procedure code. In this situation, the modifier 62 may be appended to the procedure code(s) 22548-22558 and, as appropriate, to the associated additional interspace add-on code 22585 as long as both surgeons continue to work together as primary surgeons. It represents a single complete vertebral bone with its associated articular processes and laminae. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies which contains the intervertebral disk, and includes the nucleus pulposus, annulus fibrosus, and two cartilagenous endplates. It represents a single complete vertebral bone with its associated articular processes and laminae. For the following codes, when two surgeons work together as primary surgeons performing distinct part(s) of an arthrodesis for spinal deformity, each surgeon should report his/her distinct operative work by appending the modifier 62 to the procedure code. In this situation, the modifier 62 may be appended to the procedure code(s) 22800-22819 as long as both surgeons continue to work together as primary surgeons. Non segmental instrumentation is defined as fixation at each end of the construct and may span several vertebral segments without attachment to the intervening segments. Insertion of spinal instrumentation is reported separately and in addition to arthrodesis. Instrumentation procedure codes 22840-22848 are reported in addition to the definitive procedure(s). Do not append modifier 62 to spinal instrumentation codes 22840-22848 and 22850-22852. A vertebral segment describes the basic constituent part into which the spine may be divided. It represents a single complete vertebral bone with its associated articular processes and laminae. A vertebral interspace is the non-bony compartment between two adjacent vertebral bodies, which contains the intervertebral disk, and includes the nucleus pulposus, annulus fibrosus, and two cartilagenous endplates. List 22840-22855 separately, in conjunction with code(s) for fracture, dislocation, arthrodesis or exploration of fusion of the spine 22325-22328, 22532-22534, 22548-22812, and 22830. Codes 22840-22848, are reported in conjunction with code(s) for the definitive procedure(s). Code 22849 should not be reported with 22850, 22852, and 22855 at the same spinal levels. Codes 31233-31297 are used to report unilateral procedures unless otherwise specified. The codes 31231-31235 for diagnostic evaluation refer to employing a nasal/sinus endoscope to inspect the interior of the nasal cavity and the middle and superior meatus, the turbinates, and the spheno ethmoid recess. Any time a diagnostic evaluation is performed all these areas would be inspected and a separate code is not reported for each area. If using operating microscope, telescope, or both, use the applicable code only once per operative session. Surgical bronchoscopy always includes diagnostic bronchoscopy when performed by the same physician. For endoscopic procedures, code appropriate endoscopy of each anatomic site examined.
Syndromes
- Abdominal ultrasound
- Bronchitis
- Sweating
- Developing a problem with alcohol or drugs (substance abuse). Using alcohol or other drugs increases the chances that symptoms will return.
- Do not wear jewelry, makeup, nail polish, or a wig or hairpiece.
- Abnormally high levels of red blood cells due to low blood oxygen levels
- You develop new symptoms, including side effects from the medications used to treat the disorder
- Lightheadedness
- Heart disease
- Spread of cancer to the lungs
The most likely mechanism for the hyperdynamic circulation of anemic fetuses is decreased blood viscosity vaadi herbals review order hoodia overnight delivery, leading to increasedvenous return and cardiac preload herbals wikipedia cheap hoodia 400 mg free shipping. However herbs paint and body cheap hoodia generic, severe anemia with consequent end-stage cardiac failure may be associated with high pulsatility or even reversed a wave in the ductus venosus and pulsations in portal sinus jiva herbals order hoodia paypal. The effect of replacing fetal with adult hemoglobin on the blood gas and acid?base parameters in human fetuses. Relationship of fetal hemoglobin and oxygen content to lactate concentration in Rh isoimmunized pregnancies. The relationship of fetal protein concentration and hemoglobin level to the development of hydrops in rhesus isoimmunization. Prediction of fetal anemia by measurement of the mean blood velocity in the fetal aorta. Ultrasound guided sampling of umbilical cord and placental blood to assess fetal wellbeing. Pulsed Doppler flow velocity waveforms before and after intrauterine intravascular transfusion for severe erythroblastosis fetalis. Fetal blood velocities in Rh isoimmunization: relationship to gestational age and to fetal hematocrit. In Proceedings of the Sixth Annual Meeting of the Society of Perinatal Obstetricians. Fetal cardiac output in the isoimmunized pregnancy: a pulsed Doppler echocardiographic study of patients undergoing intravascular intrauterine transfusion. Cardiac output in a fetus with erythrobastosis fetalis: assessment using pulsed Doppler. Effects of intravascular fetal blood transfusion on fetal intracardiac Doppler velocity waveforms. A comparison of sheep and human fetal oxygen delivery systems with use of a mathematical model. Cardiac changes in fetusessecondary to immune hemolytic anemia and their relation to hemoglobin and catecholamine concentrations in fetal blood. Doppler measurements of fetal and utero-placental circulation: relationship with umbilical venous blood gases measured at cordocentesis. Diagnosis of fetal anemia with Doppler ultrasound in the pregnancy complicated by maternal blood group immunization. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. The relationship between peak velocity in the fetal descending aorta and hematocrit in rhesus isoimmunization. A new splenic artery Doppler velocimetric index for prediction of severe fetal anemia associated with Rh alloimmunization. Prospective non-invasive monitoring of pregnancies complicated by red cell alloimmunization. Fetal ductus venosus blood flow velocities before and after transfusion in red-cell alloimmunized pregnancies. Fetal venous, arterial, and intracardiac blood flows in red blood cell isoimmunization. The effect of intravascular blood transfusion on the flow velocity waveform of the portal venous system of the anemic fetus. The acute effect of cordocentesis with or without fetal curarization and of intravascular transfusion upon umbilical artery waveform indices. The effect of intravascular transfusion for rhesus haemolytic disease on umbilical artery Doppler flow velocity waveforms. Effect of acute intravascular volume expansion on human fetal prostaglandin concentrations. The effect of intravascular transfusion for rhesus haemolytic disease on umbilical artery Doppler flow velocity waveforms. Increase of fetal hematocrit decreases the middle cerebral artery peak systolic velocity in pregnancies complicated by rhesus alloimmunization. Flow velocity waveforms of the vascular system in the anemic fetus before and after intravascular transfusion for severe red blood cell alloimunization. In the past, before the introduction of insulin, the main cause of death was in association with maternal keto-acidosis, but now most fetal deaths are non-keto acidotic and occur in association with fetal macrosomia. The major source of fetal glucose is the mother and there is a good correlation between maternal and fetal blood glucose concentrations 1. In pregnancies complicated by diabetes mellitus, the maternal hyperglycemia causes fetal hyperglycemia and hyperinsulinemia 2,3. Furthermore, the fetal insulin to glucose ratio is increased because hyperglycemia and/or the other metabolic derangements associated with maternal diabetes mellitus act on the fetal pancreas to cause? Fetal hyperinsulinemia causes macrosomia, either directly through its anabolic effect on nutrient uptake and utilization, or indirectly through related peptides such as insulin-like growth factors 4. Although good diabetic control in the third trimester of pregnancy reduces the incidence of macrosomia, the latter is not always preventable. In pregnant women with diabetes mellitus, despite stringent maternal glycemic control, the fluctuation in maternal glucose concentration is greater than in non-diabetics and it is possible that, during short-lived episodes of hyperglycemia, an already hyperplastic fetal pancreas will respond with a disproportionately high release of insulin. In diabetic pregnancies, analysis of blood samples obtained by cordocentesis has demonstrated significant acidemia and hyperlacticemia in the absence of hypoxemia 5-7. Fetal acidemia, which may offer an explanation for the unexplained stillbirths of diabetic pregnancies, is likely to be the consequence of increased metabolic rate. In pregnant sheep, chronic hyperglycemia results in increased aerobic and anaerobic glucose metabolism, with consequent increased oxygen consumption, lactate production and fall in pH and pO 8-13. Glucose oxidation and oxygen consumption are also increased by hyperinsulinemia, and this 2 effect is independent of that caused by hyperglycemia 12. Hyperlacticemia occurs because the fetus has a reduced capacity for oxidative metabolism and low pyruvate dehydrogenase activity. Severe hyperglycemia is characterized by acidemia and hypoxemia, but minor degrees of hyperglycemia are associated with acidemia in the absence of hypoxemia 8. However, in the presence of mild fetal hypoxemia, minor degrees of fetal hyperglycemia do result in severe acidosis and even fetal death 13. The alternative explanation for fetal acidemia in maternal diabetes mellitus is impaired placental perfusion. Histological studies have reported decreased villous surface area, villous edema and thickening of the basement membrane 14. However, the finding that acidemia is not accompanied by hypoxemia suggests that the acidemia is unlikely to be due to impaired placental function; in pregnancies complicated by intrauterine growth restriction due to uteroplacental insufficiency, acidemia is accompanied by hypoxemia (see Chapter 4). This section also examines whether impedance in the uterine and umbilical arteries can provide useful prediction of subsequent development of preeclampsia and/or intrauterine growth restriction in the same way that it does in nondiabetic pregnancies. It was suggested that, in some diabetic pregnancies, there is increased placental vascular resistance with a compensatory increase in volume flow. It was suggested that fetal heart rate variability and umbilical artery peak systolic velocity may be markers for fetal cardiovascular homeostasis in pregnancies complicated by insulin dependent diabetes mellitus 16. They found a significant association between impedance to flow and maternal serum glucose concentration. Furthermore, high impedance was associated with an increased number of stillbirths and neonatal morbidity. It was suggested that maternal hyperglycemia causes placental vasoconstriction by impairing prostacyclin production 17. In 36% of cases, there was an adverse outcome (defined as delivery before 37 weeks, or fetal risk requiring Cesarean delivery, or fetal growth restriction, or neonatal hypocalcemia, hypoglycemia, hyperbilirubinemia, or respiratory distress syndrome) 18. The higher the difference in impedance between the two uterine arteries, the greater was the risk of adverse pregnancy outcome, but there was a considerable overlap in discordance between the good and adverse outcome groups. Women with vascular disease had a higher impedance in the umbilical artery compared to those with uncomplicated diabetes. Increased impedance in women with vascular disease was associated with subsequent development of intrauterine growth restriction and, in those with no vascular disease, with the development of pre-eclampsia. Increased umbilical artery impedance was associated with the subsequent development of pre-eclampsia (in women without vasculopathy) and development of intrauterine growth restriction in those with vasculopathy.
Buy discount hoodia on line. Индийская натуральная косметика AASHA HERBALS от BlessVita.ru.