George M. Kushner, DMD, MD
- Professor of Oral and Maxillofacial Surgery
- University of Louisville School of Dentistry
- Louisville, Kentucky
Negative cognitions and beliefs about pain can lead to maladaptive coping medicine 377 generic avodart 0.5 mg otc, exacerbation of pain medications without doctors prescription buy avodart 0.5 mg free shipping, increased suffering symptoms torn rotator cuff avodart 0.5 mg low cost, and greater disability medications for adhd cheap 0.5 mg avodart with amex. Pain cognitions provide one of the most direct indicators of a patients illness perceptions and, as such, it is not surprising that a substantial number of chronic pain studies focus on the role of cognitions on chronic pain and treatment outcomes. Catastrophic thoughts or assuming the worst are among the most problematic of thought patterns associated with pain, contributing to increased pain intensity, distress, and failure to utilize adaptive coping techniques. Examples such as my pain will never stop or nothing can be done to improve my pain, may interfere with treatment. Positively, however, catastrophizing appears to respond to behavioral and cognitive behavioral interventions (Hansen, Daykin, & Lamb, 2010; Turner, Mancl, & Aaron, 2006) and may be among the most sensitive indicators of treatment outcomes. When pain is interpreted as evidence of further damage to tissue rather than an ongoing stable problem that may improve, individuals with chronic pain will report higher pain intensity regardless of whether damage is occurring (Smith, Gracely, & Safer, 1998). This belief, one of the most important among those with chronic pain, can also lead to decreased activity or inactivity. The relationship between pain and negative affect is complex and bidirectional as individuals with chronic pain are more likely to experience depressive and anxiety disorders (Bair et al. Thus combining negative affect with pain (or vice versa) operates much like turning up a volume knob or adding additional traffc on a street. Failing to accept the offered cause of pain or being unwilling to accept that a source of pain cannot be determined can interfere with effective management. Believing that ones pain is a mystery can lead to increased distress and pain intensity and can also be associated with repeated seeking of further medical tests or pursuing invasive interventions (Williams & Thorn, 1989). It involves a person achieving a level of confdence that some degree of control can be exerted over their pain. Improvements in pain self-effcacy tend to track with improvements in a variety of important pain outcomes (Turner, Mancl, & Aaron, 2006; Weitlauf, Cervone, Smith, & Wright, 2001). Behavioral Factors A high degree of variability exists in the manner in which patients behaviorally cope with chronic pain. A person can consider coping on a continuum from active to passive forms of coping. Guarding is defned as any of a set of protective behaviors such as limping, bracing, or otherwise protecting a part of the body. Guarding, similar to other pain behaviors, continues after healing has occurred and reinforces self-perceptions of disability (Prkachin, 2007). Guarding may lead to secondary problems with other parts of the body where compensation has affected alignment. Over-reliance on resting as a coping strategy can lead to deconditioning of muscles and general atrophy. Alternating rest periods with activity, also known as pacing, is a healthy way to incorporate rest. A brief explanation is included in the section below, and pacing will be discussed further in session four. Appropriate exercise and stretching can have numerous benefts for individuals with chronic pain. It can reverse the effects of deconditioning, improve strength, reduce risks associated with obesity, and decrease self-perceptions of disability. Exercise can also lead to increased stamina and increased engagement with rewarding or pleasurable activities. For some individuals, over-activity can be as problematic as avoidance of activity (Andrews, Strong, & Meredith, 2012). Individuals who routinely completely ignore pain to conduct physically stressful activities such as mowing the lawn or painting a house all at one time can pay a steep price. The overactivity may lead to infammation of pain and result in being unable to function for the remainder of a day or longer; therefore, pacing activities is recommended. As previously mentioned, pacing is the practice of engaging in an appropriate level of physical activity without signifcantly exacerbating pain (Gill & Brown, 2009). By using calculated increases in activity, pacing can lead to greater endurance and a reduced frequency of intensely painful episodes. A solicitous signifcant other is highly responsive to an individuals pain or to expressions of behavior indicative of pain (McCracken, 2005). The solicitous social interaction results in increased reports of pain as contrasted with social interactions that focus the individuals attention away from pain and onto different topics or activities. This may lead to increased pain or increased reports of disability for the person with pain (Fillingim, Doleys, Edwards & Lowery, 2003). If solicitous is at one end of the social continuum then punishing is at the other. Punishing responses involve either angry or ignoring responses, each aimed at limiting expression of pain (McCracken, 2005). Some potential consequences of punishing responses include dramatic (loud) expressions of ones pain experience in an effort to be heard or, alternately, inability to express emotions about pain can lead to stoicism and resignation. Chronic Pain Cycle Since chronic pain impacts various aspects of daily functioning and areas of life, the chronic pain cycle is helpful to understanding the process and stages that occur over time. As the fgure below illustrates, the onset of chronic pain often leads to a decrease in activities, which leads to physical deconditioning such as muscle atrophy. This fgure is used with Veterans in session 2 to discuss the impact of chronic pain. The commonality across Veterans who engage in the protocol will be the presence of chronic pain and its negative effects on their lives. The following fgure represents the cognitive behavioral model and the interaction between the clinical factors in the biopsychosocial understanding of pain. The depicted interrelationships between thoughts, emotions, and behaviors are present within most cognitive behavioral models, whereas the model below adds chronic pain. The placement of pain at the top is meant to refect its primary but also bidirectional role with all the other life factors. Behavioral experiences help show patients that they may be capable of more, physically, than they previously believed and that such gains can lead to re-engagement with rewarding experiences. Addressing negative thought patterns such as catastrophizing can help patients to view their experiences in a more balanced manner contributing to improved mood. The intervention seeks to improve Veterans reactions to the experience of chronic pain thus minimizing the negative impacts on their lives. While decreasing pain intensity is ideal, the focus is on how to reduce pain-related suffering. The authors evaluated the above questions by comparing the average effects of treatment (effect sizes) of different studies and different treatment conditions within studies. A total of 22 studies were identifed for comparison and included studies of psychological interventions for chronic pain occurring with multidisciplinary treatment or as a stand-alone intervention. Positive effects for psychological interventions, when contrasted to control groups, were identifed for pain intensity, pain-related interference, health-related quality of life, and depression. All participants received an active advisory consultation with a physical therapist with exercise recommendations. The three process studies in this section each explored potential meditational effects that operate in cognitive behavioral interventions. Smeets, Vlaeyen, Kester, and Knotterus (2006) examined whether treatments based on different theories change catastrophizing and internal control of pain, and whether such changes mediate treatment outcome. In addition to assessing the potential mediating effect of catastrophizing the study also assessed internal pain control which bears similarity to the construct of pain self-effcacy. The three active treatment groups also reported improvements in perceived disability and pain intensity. Changes in pain catastrophizing mediated the reductions in disability and pain intensity. Thus, not only cognitive behavioral treatments but also physical treatment produced changes in pain catastrophizing that also mediated general improvements among patients. Improvements in pain self-effcacy predicted the greatest level of improvement across all study outcomes. Improvements in catastrophizing also predicted a range of outcomes, although the overall impact of this variable was more modest in impact than that of the self-effcacy variable.
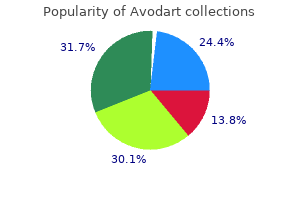
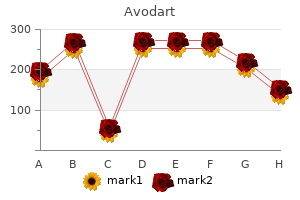
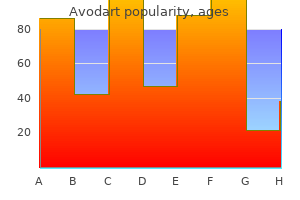
Disc material does not enhance (or has peripheral enhancement) owing to its lack of vascularity medications hair loss order 0.5 mg avodart mastercard. Pseudo-meningoceles (dura breached during surgery) - not of clinical relevance; distinguish from abscess (no communication with thecal space) medicine for the people purchase generic avodart canada. Lumbosacral adhesive arachnoiditis (intradural reactive process) - cause for failed lumbar disc surgery - occurs in only 3%; markedly diminished since abandonment of preoperative myelography using oil-based iophendylate (Myodil medications japan travel buy avodart uk, Pantopaque) medicine jewelry order avodart no prescription. Avoidance of certain activities (bending or twisting at waist frequently, lifting heavy objects). Detach scar tissue from dura using curette (same if disk fragment is attached to dura) ? always stay on bone (the only safe way). Patients in tubular diskectomy arm had significantly inferior patient satisfaction scores with microtubular diskectomies versus traditional open microdiscectomies. Core can be: A) mobile (unconstrained) B) fixed to one of the end plates (constrained) biomechanical studies show no significant advantage of constrained (ProDisc-L) over an unconstrained device (Charite). Caudal or medial penetration of pedicle cortex can result in dural or neural injury (nerve root occupies ventral and rostral one-third of foramen). Extensive tissue dissection (to expose entry points + to provide required lateral to medial orientation for optimal screw trajectory) > costly lengthy operation, significant blood loss. Painful spinal instability: 1) post-laminectomy spondylolisthesis 2) painful pseudoarthrosis 2. Definition of instability, Principles of spondylolisthesis treatment Indication for fusion ? (predisposition for) instability! Direct surgical decompression alone may be considered for symptomatic stenosis associated with low grade degenerative lumbar spondylolisthesis when symptoms have been recalcitrant to a trial of medical/interventional treatment (grade of recommendation: C). Fusion is suggested to provide long term clinical improvements (grade of recommendation: B). Insufficient evidence to indicate that fusion leads to improved long term outcomes as compared with a directed exercise program. Insufficient evidence to recommend one surgical fusion technique over another to improve long term outcomes. For low-grade isthmic spondylolisthesis, the addition of instrumentation to posterolateral fusion may not improve outcomes (grade of recommendation: B). Insufficient evidence to make a recommendation regarding which prognostic factors have been associated with good or poor surgical outcomes. Screw pullout resistance: major screw diameter thread depth - screw pullout resistance is proportional to volume of bone between threads. Only disadvantage ? if patient will need revision in the future, the larger diameter screws may be needed! Pressurized injection of polymethylmethacrylate into screw hole causes acrylic to penetrate into bony interstices (G) - this effectively increases screw diameter (H). Mathern uses mamillary process gift of nature as entry point (thus, dissect that area thoroughly to see bone anatomy). Mathern) **curved tip is facing laterally (to avoid medial breech) and, once passed pedicle, flipped to face medially thoracolumbar junction (Th10-L2) pedicles are almost strictly sagittal (or 3-5 degrees per Dr. A - pedicle width B - transverse (coronal) pedicle angle C - sagittal pedicle angle Transverse pedicle angle, s. Sagittal pedicle angle increases from 0? at T1 to 10? at T8 and then decreases to 0? at T12. Optimal triangulation effect that accommodates forces applied in all planes is 90 degrees (C). Long segment fusions to the sacrum, particularly in patients prone to L5-S1 pseudarthrosis, such as patients with global or lumbar sagittal imbalance or bony deficiency. Spondylolisthesis (symptomatic, progressive, or requiring decompression that necessitates stabilization) 2. Pseudarthrosis of previous intertransverse fusion that requires fusion technique with higher success at achieving solid arthrodesis 4. Osteoporotic end plates that may not hold interbody graft, leading to subsidence 2. Smith-Peterson osteotomies or removal of Gill fragments) can be performed for greater exposure of nerve root and disk space + unroofing neural foramen + allows compression of screws / disk space perform annulotomies on both sides with No. Complications 1) implant migration - observed in majority of patients 2) retrograde ejaculation and sterility (1-5%) - from injury of superior hypogastric sympathetic nerve plexus (particularly when operating at L4/L5); H: avoid using Bovie (use bipolar! Posterior enforcement supplemental posterior percutaneous pedicle screws lead to comparable clinical outcomes to those undergoing open posterior instrumentation. The spinous process and facets of the upper vertebra are removed in addition to the superior facets of the inferior vertebra; areas to be removed are painted in red. Technique: instrumentation should be done before any osteotomy attempt - standard pedicle screws are used at least three levels above and below the level of osteotomy. Otherwise, when there is a fused spine above and below the osteotomy line, as in ankylosing spondylitis or previous fusion cases, as the rod is not as acutely angulated as the spine, it does not sit into the grooves and pulls the screws just above and below the osteotomy line and causes loss of correction. Note that a wedge reaching to , but not crossing, the anterior cortex is to be removed. The parts of the laminae painted in red may be preserved if they do not interfere with closure of the osteotomy gap. Again, the area painted in red may not be removed if enough decompression is done and these structures do not prevent closure of the osteotomy. Technique pedicle screws are placed at least two levels below and three levels above the planned osteotomy level, followed by wide laminectomies of the vertebrae above and below the disc space planned to be resected. Upper end-plate of T10 and lower end-plate of T9 were included in the area to be resected. Lower facets and spinous process of the upper vertebra and upper facets of the lower vertebra should be removed to gain access to the area to be resected. Lower facets of the upper and upper facets of the lower vertebrae should be removed to allow removal of the laminae and pedicles of the vertebra to be resected. Discs should also be resected and this should be followed by end-plate preparation for a successful fusion. Circumferential wedge bone resection - variant with wedge-shaped apical vertebral body bone resection in addition to apical laminectomy and laminectomies of vertebrae directly superior and inferior to apex; apical facets and pedicles are removed completely. This allows hinging to be over posterior vertebral body rather than anterior cortex, resulting in greater correction. Its short-term and long-term effects in the operation time, intraoperative blood loss, post- treatment of lower lumbar degenerative disease operative drainage volume, blood transfusion are also superior. There were no signifcant differences be- from one side for bilateral interbody fusion. At the same time, in passage tube minimally-invasive system, such as order to further increase the convenience of op- Quadrant system, establishes the surgical chan- eration and reduce the radiation exposure during nel using the step-by-step expansion method, operation, we designed the special retractor and exposing limitedly and minimizing the tissue fxation guide device based on the characteristics damage in surgical approach and surgical pro- of new approach, making the operation simpler cedures. Compared with the conventional open and more convenient and reducing the radiation surgery, it can not only complete the operation, exposure17,18. Inclusion criteria: 1) patients with lower operation, too long learning curve, early cerebro- lumbar pain accompanied with radiating pain in spinal fuid leakage, high misplacement rate of lower limbs and intermittent claudication; 2) pa- pedicle screw, combination with percutaneous12 tients who were not improved after conservative fxation technique, much radiation exposure re13 - treatment; 3) patients diagnosed as single-seg- quired during operation, high cost of operating ment lesion, including lumbar instability, pure apparatus and supporting implantation materials protrusion of intervertebral disc, degenerative and repeatedly slipped muscle in channel opera- lumbar stenosis, fbrous ring prolapse and lum- tion, so in order to ensure the clear surgical feld bar spondylolisthesis, according to preoperative sometimes, spine surgeons often choose cauteri- physical examination, combined with lumbar zation and partial resection of muscle14,15. Exclusion criteria: patients with more imally invasive characteristics of channel tech- than one-segment lesion who needed operation; nique and overcome the shortcomings of channel patients with a history of mental illness; patients technique, we modifed the Wiltse approach a with a history of lumbar surgery; patients with second time in the preliminary study. The skin was cut medical diseases; patients with severe osteoporo- along the supraspinous ligament subcutaneously sis (T-value -2. This study was approved by the Ethics Com- skin was separated along the bilateral multifdus mittee of Taizhou Peoples Hospital affliated muscle and deep fascia to the space between mul- to Nantong University. Signed written informed tifdus and longissimus muscles until the lateral consents were obtained from all participants be- border of facet joint. The physical examination of all patients must be For patients with obvious facet hypertrophy, the consistent with the results of imaging examina- osteophyte should be removed properly to expose tion. After operation, the placement of pedicle the articular surface and further clarify the lateral screw and interbody fusion cage was detected border of upper joint. The conventional fuoroscopic ex- Under conventional general anesthesia, eye- amination was generally performed after the frst glass frame -like locator was used to position guide pin was inserted to determine if the surgi- the intervertebral space and pedicle via modifed cal segment was correct, and then fuoroscopic intermuscular space approach, and the median in- examination was not needed in the subsequent cision between upper and lower vertebral pedicles operation (Figure 2). Decompression and inter- was made with the length of about 5 cm-6 cm body fusion treatment: According to the patients (Figure 1). Generally the incision was extended symptoms and signs, those with severe symptoms towards the head side, so as to place the screw in both lower limbs were treated with interbody and fusion cage easily (the placement of lower fusion cage for bilateral decompression, but the 55 H. A, Screw fxation via the unilateral intermuscular space assisted by the retractor; B, Bilateral deep fascia and spinous process were sutured together to close the incision; C, Well-pre- served multifdus muscles on both sides; D, Length of surgical incision; E, Single-segment patients receiving bilateral decom- pression, intraoperative blood loss of 280 mL. Even in the bilateral decompression, was routinely implanted into the intervertebral the spinous process and supraspinous ligament were space.
Historically symptoms of hiv buy discount avodart 0.5mg online, non-union realise that disc degeneration is symptomless in the (pseudoarthrosis) was a common problem with majority of cases and this may only lead to symptoms of uninstrumented spinal fusion treatment arthritis buy 0.5 mg avodart with amex. Nowadays symptoms 7 days after ovulation discount avodart 0.5mg mastercard, pain symptoms 4 weeks pregnant cheap 0.5mg avodart fast delivery, but also leg pain (sciatica) secondary to disc pedicle screws are wildly employed in posterior herniation, spinal canal stenosis, and spinal deformities. Such non-surgical options should 1953), has been the most popular posterior technique. A disadvantage of this technique, as compared to Spinal fusion/spinal arthrodesis anterior techniques, is that it can produce more neurological Spinal fusion has been practiced since the beginning of complications, bleeding, and subsequent scar formation the 20 century and was mainly used for spinal deformitiesth within the spinal canal (Krishna et al. Today, fusion is the by Harms and Rolinger and offers the advantage of most commonly performed spinal operation. Concerns include more serious of low back pain and the limited and inconsistent success complications such as vascular lesions, and in the of spinal fusion, indications for surgery vary between lumbosacral junction, injury to the presacral plexus can countries and surgeons (Fritzell et al. More complex techniques use an anterior approach controversial with conflicting results (Gibson et al. Arrows show the posterolateral autologous bone graft (B) Lateral view of the same patient. Arrows show the radio-opaque markers embedded in the cages that have been filled with bone graft. Results have varied, with fusion not proving its superiority as compared to placebo or non-operative treatment (Gibson et al. A multi-centred randomised trial performed in Sweden nevertheless, provided evidence that surgery may be more effective than non-surgical treatment in patients suffering with low back pain secondary to degenerative disc disease (Fritzell et al. A study by a Norwegian team however, failed to show the superiority of surgery if conservative treatment was carried out using a more intensive approach including cognitive intervention (Brox et al. Furthermore, long-term consequences such as adjacent segment disease have also increased concerns for the use of spinal fusion (Gillet, 2003; Okuda et al. Several changes have been observed such as dehydration, disc space narrowing, osteophyte formation and progressive deformity at levels adjacent to a fused spinal segment (Gillet, 2003). Given the debatable efficacy of spinal fusion and its possible implication in the degeneration of the adjacent segments, various non-fusion techniques have been developed. Attempts have been made since the 50s to produce an implant that can mimic, to some extent, the function of the Fig. The surgical approach is similar to the one used to obtain an anterior lumbar interbody fusion and carries similar rates of vascular complications. Similar to spinal fusion, some of the indications for total disc replacement include failure of aggressive conservative treatment with disabling low back pain attributed to degenerative disc disease of the lower lumbar spine affecting no more than two discs. Thus, intact facet joints posteriorly are thought to be a prerequisite (Fekete and Porchet, 2010; Kishen and Diwan, 2010). Furthermore, this technique does not those with anterior lumbar interbody fusion (Blumenthal address degenerative changes that may already be present et al. Different designs present different challenges but, in general, nuclear replacement designs must resist migration, avoid subsidence, as well as manage the risk of device expulsion. The latter can be either made of a hydrogel or a non-hydrogel substance, and are available in injectable or pre-formed shapes (Coric and Mummaneni, 2008). Nevertheless, this nuclear replacement has not been primarily used for low back pain, but as an adjunct to disc surgery following removal of the nucleus in cases of disc herniation. So far, several thousands of these implants have been used in clinical practice and although initially there were concerns of dislodgement, modification to the design has improved safety. Dynamic stabilisation With a view to address some of the shortfalls of spinal fusion, alternative options for the last decade have included the use of semi-rigid or dynamic stabilisation implants. Semi-rigid stabilisation aims to achieve fusion without stress shielding at the bone graft that may disrupt or delay Fig. The Graf consists a non-elastic band spondylolisthesis or scoliosis following decompression sometimes referred to as a prosthetic ligament that is (Schaeren et al. In terms of clinical outcomes, attached between pedicles screws, placing the motion results from the literature are mixed. Results from Beastall segment to be stabilised in lordosis (Mulholland and and colleagues confirm that the Dynesys allows movement Sengupta, 2002; Huang et al. The idea behind this of the instrumented level without significant increases in concept was that the device would limit flexion to within motion at the adjacent levels (Beastall et al. Although the Graf device showed contrast, results from a more recent study by Cakir and significant clinical success (Grevitt et al. The support for the use of the Dynesys as compared to fusion design of the Dynesys is similar to the Graf with the (Grob et al. The same study also found relatively exception that it has an additional polycarbonate-urethane high reoperation rates after use of the Dynesys device. Thus, in addition to the band limiting fusion) for the treatment of degenerative disc disease. Disc degeneration: current surgical options Unlike the aforementioned Graf and Dynesys that are fixed to the vertebrae by the use of pedicle screws, interspinous implants are floating devices with the advantage of limiting the possibility of loosening during motion (Sengupta, 2004). Similar to dynamic stabilisation devices and classified as such, their basic design aims to avoid excessive extension and unload the posterior annulus, which is regarded as the primary pain source. Different designs however serve different indications, some limiting flexion and/or extension. Interspinous devices consist of either compressible or non-compressible implants (Fig. They are usually introduced through a minimal invasive approach between the spinous processes of the affected level. This technology again has not been studied in a prospective randomised way, at least as far as treating discogenic low back pain is concerned. Nevertheless, there have been studies evaluating the efficacy of such devices in a different setting, namely that of spinal stenosis, in which there appears to be some effectiveness, albeit limited in time (Zucherman et al. It involves inserting a navigable electrothermal catheter to the inner posterior annulus and delivering heat that aims at inducing retraction of the annular collagen, therefore coagulating inflammatory tissue and nerve endings in the periphery of the disc posteriorly (Saal and Saal, 2000). Although somewhat difficult to achieve, placement of the electrothermal catheter should aim to allow for the active portion of the catheter to provide sufficient heat to spread to both the outer and inner annulus (Karasek and Bogduk, 2000; Derby et al. Lateral view of the lumbar spine showing two pain after at least 3 months of aggressive conservative non-compressible interspinous devices implanted at the treatment, normal neurological examination, less than 30% L3-4 and L4-5 levels. One study noted no statistically or clinically program including some type of cognitive intervention. Interspinous devices are only employed in eds), 3 edn, Lippincott Williams & Wilkins, Philadelphia,rd selected spinal stenosis cases but due to the lack of evidence pp 317-323. Clin Orthop Rel Low back pain is a multi-factorial problem affecting a great Res 394: 139-145. Thus, treatment of low Beastall J, Karadimas E, Siddiqui M, Nicol M, Hughes back pain resistant to conservative management is still a J, Smith F, Wardlaw D (2007) the Dynesys lumbar spinal very complex issue. The currently available surgical stabilization system: a preliminary report on positional options are moderately effective with the majority of them magnetic resonance imaging findings. It is therefore not surprising Bertagnoli R, Kumar S (2002) Indications for full that surgeons are looking towards more physiological prosthetic disc arthroplasty: a correlation of clinical solutions, and this is where translational multidisciplinary outcome against a variety of indications. Eur Spine J 11 collaboration between clinicians and researchers may offer Suppl 2: S131-S136. Current research in biological solutions Bertagnoli R, Karg A, Voigt S (2005a) Lumbar partial focusing on either protein injections (e. Indications, Clinical experience with the Dynesys semirigid fixation operative technique, after care. Lippincott Williams & Wilkins, Philadelphia, Hannani K, Delamarter R (2004) Operative treatment pp 393-398. Pathophysiology of lumbar disc degeneration: a review of In: the Lumbar Spine (Herkowitz H, Dvorak J, Bell G, the literature. Clin Orthop Rel Res 335: randomized trials comparing lumbar fusion surgery to 39-53. A comparative biochemical, histologic, lumbosacral fusion: review of the literature. Activity level on the other of pedicle screw/plate fixation on lumbar/lumbosacral hand has to be taken into account. In active young athletes, autogenous bone graft fusions in patients with degenerative spinal fusion of a single level, in particular of the lesser disc disease. Anterior surgery Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, would be technically more complex in such patients and Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers thus the senior author would prefer a more conservative T, Sachs B, Girardi F, Kropf M, Goldstein J (2007) Results posterior technique. Which fusion for the treatment of 1-level degenerative disc treatment options would thus be more promising than disease. For more advanced degeneration, including annular degeneration and secondary facet joint changes, a more drastic approach Discussion with Reviewers may be needed.
Syndromes
- Swelling of the abdomen
- Rosacea
- Diarrhea
- Disorders of the testicles, ovaries, or adrenal glands
- Stiffness or tightness of the arch in the bottom of your foot.
- Diazoxide (Hyperstat)
- Weakness
- Confusion
- Pulmonary infections
- "Butterfly" rash across bridge of nose and cheeks
The operative risks are much the same as with the posterolateral approach with a higher risk of injury to the dura and the added risk of injury to retroperitoneal organs at the upper lumbar levels treatment goals for ptsd purchase avodart line. Endoscopic Approaches To the Cervical Spine Anterior Approach the anterior approach is very similar to the traditional microsurgical approach with the neurovascular sheath being positioned lateral to the working channel and the visceral structures medial to the working channel medications ending in pril order genuine avodart online. The tip of the working sleeve is positioned against the anterior longitudinal ligament and the edge of the anterior part of the adjacent vertebral bodies treatment zamrud 0.5 mg avodart with visa. While traditional microsurgery requires a discectomy medications that cause hyponatremia buy avodart in united states online, traversing the disc space with an endoscope requires the resection of only a small amount of disc tissue. Sequestrectomy and when required removal of osteophytes is achieved by using a wide range of special instruments including burrs, trephines, microresectors, various types of forceps, drills, hooks and bipolar microelectrodes. By means of this approach, the foraminal areas and the spinal canal, but not the interpedicular space can be reached with excellent control of the operating field. More so than in the other segments of the spine, the anterior endoscopic approach facilitates the effective anatomical decompression of the spinal canal and/or the nerve roots (plus in select cases even the vertebral artery) without the requirement to replace the disc by means of a fusion or an arthroplasty. Posterior Approach the posterior approach is very similar to the traditional microscopic-assisted keyhole-foraminotomy approach, just that it is performed using endoscopic equipment and through a smaller approach. However, adequate experience in endoscopy and bone resection with drills is necessary due to the risks and consequences of damaging the central nervous system. After insertion of the working sheath and the endoscope, preparation of the medial aspect of the facet joint and of the ligamentum flavum is performed to clearly identify the anatomical landmarks. The foraminotomy is begun by bone resection at the medial aspect of the facet joint, resection of the lateral ligamentum flavum. Then, the lateral edge of the spinal cord and the branching spinal nerve are identified. Bone resection is necessary in nearly all cases and is performed under direct visual control using drills and bone punches, inserted through the endoscopes working channel. Bipolar radiofrequency coagulation of the epidural venous plexus and preparation of the spinal nerve under particular attention to possibly separate motor and sensory fascicles comes next. Depending on the pathology in the individual case, the foraminotomy can be extended towards lateral or cranio-caudal. At the ends of the procedure, direct closure of the skin is done and no drain is required. Complications While recent studies have shown that endoscopic spinal surgery can be performed with lower complication rates than microsurgical spine surgery, the complications of minimally invasive spine surgery are not necessarily minimal when they do occurr. Also, the learning curve for endoscopic spinal surgery tends to be flatter and longer than for traditional approaches. Dural tears, nerve root damage, bleeding and infection, operating on the wrong level or on the wrong side are as real with endoscopic techniques as they are with open techniques. In addition, some injuries may be underestimated or even go unnoticed, such as a dural tear under the low-pressure irrigation of an endoscopic system. Meticulous selection of suitable cases, careful surgical technique, perioperative single- shot antibiotics [1] and careful postoperative follow-up are therefore strongly recommended when a surgeon begins to perform endoscopic spinal surgery. When complications occur, they need to be addressed in the same way as with open surgery and, if required, by conversion to an open technique. On the one hand, such experience is required for being able to manage potential complications in an adequate fashion. On the other hand, surgeons experienced in both techniques will be able to appropriately decide in which individual cases an open approach might be better and safer than an endoscopic approach and vice versa. Adequate training in endoscopic techniques and technical versatility with the instruments to be used need to be acquired prior to independently performing such procedures in a clinical situation. Evidence Why We Need It Considering the great interest in this key question, there is surprisingly little hard proof, that minimally invasive spine surgery not only produces smaller incisions, but that it has measurable and clinically relevant advantages over more invasive, more open procedures that serve the same goal. While some evidence to that effect has accumulated during recent years, most if not all of the observed advantages relate to perioperative and early postoperative parameters. As of yet, no study has shown an advantage in mid- or long-term outcome, which runs parallel to what has been observed with the minimally invasive techniques in hip arthroplasty surgery. Still, less tissue damage, less blood loss, less postoperative pain, early mobilization and smaller incisions are advantages ? as long as they do not come at the cost of increased risks. Some proponents of the standard techniques are making the case, that because endoscopic spine surgery is currently very much en vogue, long and flat learning curves arent openly mentioned and complications are underreported [2]. The easy reply would be, that such claims can be made against any new or established surgical technique, many of which dont rest on a solid basis of evidence. However, in the best of our patients interest and while further developing endoscopic spine surgery, we must objectively evaluate its value against standard techniques. And amongst the parameters studied, the rates and the gravity of complications if they occur are at least as important as pain scales and functional scores. Systematic Reviews A 2002 systematic review by Maroon concluded that none of the minimally invasive techniques that have been developed for the treatment of symptomatic lumbar disc disease has yet been demonstrated as being superior to microdiscectomy [3]. The 2007 update of the Cochrane Collaborations systematic review on surgical interventions for lumbar disc prolapse found that surgical discectomy (open and microsurgical) for carefully selected patients with sciatica provides faster pain relief than conservative treatment [4]. The most recent systematic review on the topic was published in 2009 and it found the open, the microscopic and the endoscopic posterior discectomy surgical techniques equally effective [5]. So clearly there is a need for well-designed randomized trials comparing endoscopic techniques to the respective standard techniques, where possible. Randomized Controlled Trials A large number of clinical papers on endoscopic spinal procedures report on case series, technical innovations or personal experience. In recent years, however, several controlled and randomized controlled studies have been published which provide evidence on endoscopic spine surgery. Physiological and Biological Studies On Minimal Invasiveness An early study on 15 patients compared pulmonary function and body temperature in patients undergoing open laminectomy and discectomy to that of patients undergoing microdiscectomy [13]. It found significantly depressed pulmonary function for 20 hours post surgery and febrile temperatures for 48 hours post surgery in patients operated on with the open technique but not in patients undergoing microdiscectomy. A controlled trial comparing endoscopic and open technique found significantly less intraoperative nerve root irritation with endoscopy by means of intraoperative electromyographic monitoring [15]. Summary Randomized controlled trials have demonstrated equal effectiveness of the endoscopic procedures compared to the microsurgical reference procedures in cervical as well as in lumbar applications. Some of these studies also showed lower complication rates with endoscopy and none had higher complication rates with endoscopy. In these trials, spinal endoscopy generated less postoperative pain and faster rehabilitation than the microsurgical procedures. However, all these trials with one exception were performed by the same team of highly experienced endoscopic spinal surgeons. It is conceivable, that surgeons with less experience may not necessarily be able to achieve the same results. Sofar, no long-lasting advantages of endoscopic spine surgery over the microsurgical technique have been demonstrated. There is some experimental evidence that the effects of reduced access trauma can be measured, but interestingly, there seems to be no advantage of using a microtubular retractor system over standard microsurgical technique and instruments. Gotfryd A, Avanzi O (2009) A systematic review of randomised clinical trials using posterior discectomy to treat lumbar disc herniations. Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5. Ruetten S, Komp M, Merk H, Godolias G (2009) Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Ruetten S, Komp M, Merk H, Godolias G (2009) Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. A comparison study of microsurgical lumbar discectomy with standard lumbar discectomy. Percutaneous (endoscopic) decompression discectomy for non-extruded cervical herniated nucleus pulposus. Percutaneous microdecompressive endoscopic cervical discectomy with laser thermodiskoplasty. Percutaneous endoscopic cervical discectomy for discogenic cervical headache due to soft disc herniation. Transforaminal percutaneous endoscopic lumbar discectomy for upper lumbar disc herniation: clinical outcome, prognostic factors, and technical consideration.
Purchase avodart online pills. MY TREATMENT | LEMTRADA | MY MS STORY.